Innovative approaches are transforming medical monitoring into a strategic and proactive discipline. Medical Monitors act as expert consultants to sponsors and project teams, safeguarding participants while guiding trials to smoother execution. Critical, data-informed monitoring is now essential for ensuring compliance, quality, and trial success.
Beyond SOPs to Innovation
Strategic monitoring means reframing the roles of Medical Monitors from a regulatory necessity into a lever for innovation. It hinges on combining deep clinical expertise with operational foresight. For example, the traditional Medical Monitoring Plan has evolved into a dynamic tool that adapts to the trial’s changing needs.
Guidelines such as ICH E6(R3) are reinforcing this shift, promoting continuous, risk-based oversight powered by real-time data. This proactive posture transforms Medical Monitors into contributors to protocol design and regulatory strategy, rather than responders to emergent issues.
Proactive Planning for Patient-Empowered Trial Success
Effective medical monitoring begins long before the first patient is enrolled. Medical experts contribute to strategy development, feasibility assessments, protocol review, and therapeutic training, ensuring protocols are realistic, patient-empowered, and aligned with clinical standards. Early engagement prevents issues such as impractical procedures or restrictive eligibility criteria that can delay enrollment or trigger amendments.
As trials progress, continuous oversight allows Medical Monitors to detect emerging safety signals and protocol deviations early, enabling rapid, targeted intervention. This approach is especially critical in early-phase trials, where risks are less predictable and timelines are compressed. Early and ongoing medical engagement leads to safer trials, reduced delays, and stronger outcomes.
Precision Through People
At the heart of effective monitoring are skilled multidisciplinary medical teams with cross-functional agility and deep expertise in specific indications. Matching monitor capability to study complexity ensures that the right insights are available at the right time.
Strong site relationships further enhance compliance and performance. Monitors provide real-time support to investigators, ensuring that safety protocols and eligibility criteria are applied consistently and correctly. This human collaboration builds trust across all stakeholders.
Medical Monitoring Excellence Across Studies
Medical monitoring must adapt as trials progress or as demands arise:
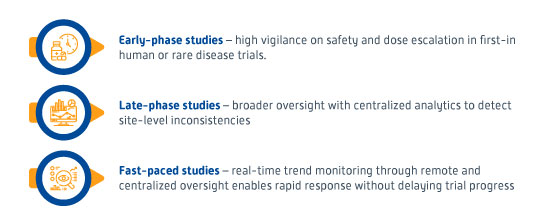
By tailoring oversight intensity and focus to each trial phase and context, minimal disruptions occur while protecting patients’ safety and data integrity.
Synchronizing Data for Metrics-Driven Monitoring
Medical monitoring demands seamless integration with the Pharmacovigilance and Data Management teams. Rather than siloed operations, Medical Monitors should collaborate with safety and biometrics groups to form a cohesive, real-time view of trial health.
This approach involves aggregating clinical, safety, and laboratory data to detect cross-domain signals, enabling faster interventions and more coherent regulatory reporting. It not only strengthens patient safety but also aligns with regulators’ push for holistic, risk-based oversight. When combined with human clinical expertise, integrated systems ensure that nothing is overlooked—even in data-heavy, complex trials.
The shift from checklists to intelligent, outcome-focused metrics enables Key Risk Indicator (KRI) assessment that reflects actual clinical impact. Metric scores inform real-time decision-making, while feedback loops drive ongoing improvement.
This data-driven mindset extends to tailoring strategies based on the type of trial. Often, the benchmark is across indications and phases, adjusting oversight based on complexity and risk. The result is a more innovative and adaptable monitoring engine that enhances transparency, speeds execution, and improves compliance.
Conclusion
Medical monitoring is evolving, from reactive oversight to predictive, patient-focused strategy. With advanced analytics and AI augmenting clinical judgment, Medical Monitors can anticipate emerging trends before they escalate, to safeguard participants and reduce trial disruptions. Ultimately, proactive, metric-driven monitoring is more than a safety measure. It ensures smoother trials, stronger data, and greater confidence in regulatory readiness.
About ClinChoice
With over three decades of global experience, ClinChoice has been at the forefront of transforming clinical development through precision, agility, and scientific rigor. Our deep roots in medical monitoring give us the insight to anticipate challenges and the expertise to design solutions that protect patients and accelerate outcomes. Backed by a legacy of trusted partnerships and regulatory excellence, ClinChoice brings an unmatched perspective to today’s complex trials, turning data into foresight and oversight into innovative strategies.
About the Author
Dr. Irina C. Pavel-Knox
Senior Director, Medical Monitoring
Dr. Pavel-Knox is an accomplished physician and the Head of the Medical Monitoring Team at ClinChoice. With over two decades of experience in medical research, she has served as Principal Investigator in more than 50 clinical trials and has played a pivotal role in numerous Phase I–IV studies as a Medical Expert. Prior to her current role, Dr. Pavel-Knox provided both medical and surgical care in major university hospitals across the UK. She holds particular expertise in respiratory research and is an active member of the European Respiratory Society.
