In longitudinal clinical trials, missing data is a threat to scientific integrity. Whether due to patient dropouts, missed visits, or protocol deviations, these gaps can distort results, reduce statistical power, and invite regulatory scrutiny. With dropout rates averaging around 3-8% for the last three years, the stakes are high. As the industry continues to evolve, so should the strategies we implement.
The Fall of Traditional Fixes
For years, researchers have relied on methods such as Complete-Case Analysis (CCA), Last Observation Carried Forward (LOCF), and Baseline Observation Carried Forward (BOCF). These approaches were simple, but simplicity came at a cost: bias, reduced precision, and regulatory disapproval. LOCF, for instance, assumes no change after dropout—a dangerous assumption in trials where patient conditions fluctuate. Mean imputation is another outdated fix, which artificially narrows confidence intervals by pretending missing data doesn’t exist.
Regulators, such as the EMA and FDA, have taken a firm stance and now discourage these methods, urging investigators to adopt more principled approaches that reflect the uncertainty introduced by the missing data.
Modern Solutions: Statistical Tools That Work
Today’s gold-standard methods embrace complexity and uncertainty, offering robust alternatives to outdated fixes.
Mixed Models for Repeated Measures (MMRM)
MMRM uses maximum likelihood estimation to handle missing data under the “missing at random” (MAR) assumption. It models correlations over time and retains precision, making it a preferred choice over LOCF in primary analyses.
Multiple Imputation (MI)
MI follows Rubin’s three-step framework: impute, analyze, and pool. It generates multiple plausible datasets, preserving variability and offering more valid inferences than single imputation. MI is flexible, accommodating arbitrary patterns and covariates, and is widely accepted in regulatory circles.
Going Deeper: Handling MNAR and Complex Dropout Patterns
When data are “missing not at random” (MNAR)—say, when patients drop out due to worsening symptoms—standard methods fall short. That’s where advanced models come in.
Pattern-Mixture and Selection Models – These models stratify data by dropout patterns or jointly model dropout and outcomes. Control-based imputation, for example, assumes dropouts follow the control group’s trajectory, which is a conservative but insightful approach for sensitivity analysis.
Delta-Adjustment Imputation (or Tipping Point Imputation) – This is a sensitivity analysis method for handling missing not at random (MNAR) data by systematically adjusting imputed values to explore how different assumptions about the missing data mechanism might affect study conclusions. In practice, a “delta” (a constant shift) is added to or subtracted from the imputed values relative to the observed data or a reference group, allowing investigators to assess how robust results are to increasingly unfavorable or favorable assumptions about the missing outcomes. When applied across a range of deltas, this approach creates a “tipping point” analysis that identifies the point at which study conclusions (e.g., treatment efficacy) would change, offering valuable insights into the potential impact of MNAR mechanisms.
Bayesian Methods – Bayesian frameworks integrate expert priors and historical data, using posterior distributions and MCMC (Markov Chain Monte Carlo) to impute missing values. They’re ideal for adaptive trials and small samples, offering nuanced insights where traditional methods struggle, like the null hypothesis significance testing and frequentist methods.
Inverse Probability Weighting (IPW) – IPW adjusts for dropout by weighing observed data based on dropout probabilities. While useful under MAR (missing at random), it’s sensitive to model specifications and less stable in small samples.
Design Strategies to Minimize Missingness
Prevention is better than cure. Thoughtful trial design and operational practices can drastically reduce missing data.
Protocol-Level Planning
- Simplify trial procedures to reduce participant burden.
- Offer remote or flexible visit options.
- Inflate sample size to account for expected attrition.
- Continue follow-up even after treatment discontinuation.
Operational Practices
- Pre-specify missing data handling in protocols and SAPs.
- Use clear consent forms to set expectations.
- Collect reasons for dropout to inform analysis and future design.
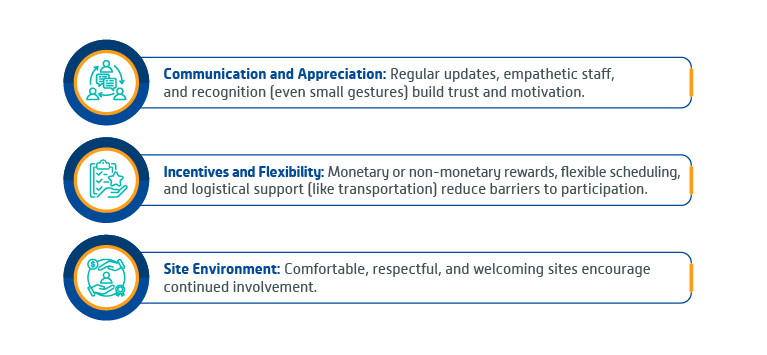
Keeping Participants Engaged: Retention as a Data Strategy
Engagement isn’t just ethical—it’s strategic. Trials that prioritize participant experience see lower dropout rates.
Monitoring and Reacting in Real Time—Aligning with Regulatory Expectations
Real-time data capture systems flag missing entries instantly, allowing for prompt follow-up and ensuring data integrity. Centralized monitoring helps identify dropout trends, while re-engagement tactics like rescheduling visits can recover data and maintain participant relationships. Regulatory bodies require trials to plan for missing data from the start. The ICH E9(R1) framework emphasizes defining treatment effects and strategies for intercurrent events, making sensitivity analyses essential to validate conclusions under various assumptions, especially when data is MNAR.
Conclusion
Handling missing data isn’t just about plugging gaps. It’s about preserving the integrity of clinical evidence. By combining proactive design with robust statistical methods, researchers can ensure their findings withstand both scientific and regulatory scrutiny. The message is clear: plan ahead, engage participants, and use the best tools available. Because in clinical trials, what’s missing can matter just as much as what’s observed.
About the Author
Jianrong Li
Vice President, Biostatistics and Programming
With extensive expertise in statistical consultation and strategic leadership, Jianrong guides the Biostatistics group through all phases of drug development, from planning to execution. A trusted authority in statistical and programming methodologies, he offers direction to teams while driving corporate-level initiatives. Additionally, he plays a pivotal role in business development and fostering strategic client partnerships, ensuring the seamless integration of science and strategy at every stage of the drug development process.
